CPT code diaphragmatic hernia repair embarks on an insightful journey, delving into the complexities of this surgical procedure. From its preoperative considerations to postoperative care and long-term outcomes, this article provides a comprehensive overview of diaphragmatic hernia repair, shedding light on its nuances and significance in surgical practice.
Diaphragmatic hernias, characterized by the protrusion of abdominal contents through an opening in the diaphragm, pose a significant health concern. This article explores the various types of diaphragmatic hernias, their causes, and the clinical presentation associated with each type.
Overview of Diaphragmatic Hernia Repair
Diaphragmatic hernia refers to an abnormal opening in the diaphragm, the muscle that separates the chest cavity from the abdominal cavity. This opening allows abdominal organs, such as the stomach or intestines, to protrude into the chest cavity.
- Causes:Diaphragmatic hernias can be congenital, present at birth, or acquired later in life due to trauma or increased pressure on the diaphragm, such as from obesity or pregnancy.
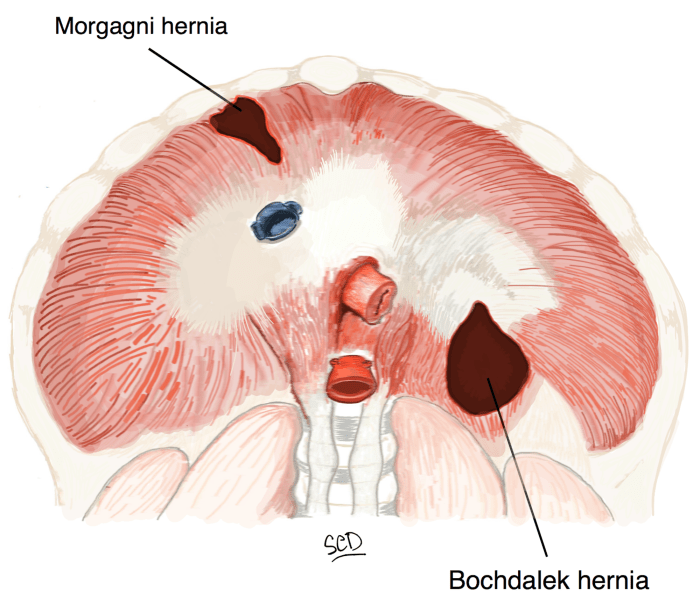
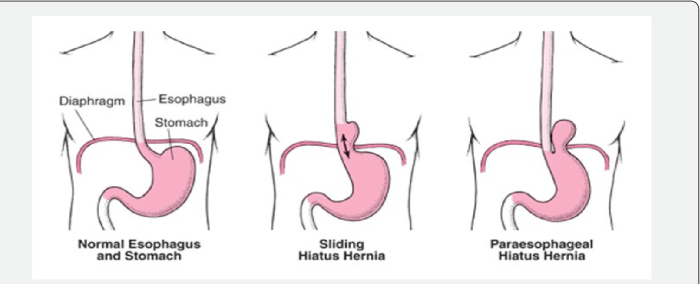
- Types:There are different types of diaphragmatic hernias, classified based on their location and the organs involved. Common types include:
- Hiatal hernia:The stomach protrudes through an opening in the diaphragm called the esophageal hiatus.
- Morgagni hernia:An opening in the anterior portion of the diaphragm allows abdominal contents to enter the chest cavity.
- Bochdalek hernia:A defect in the posterior portion of the diaphragm allows abdominal organs to enter the chest cavity.
- Symptoms:Diaphragmatic hernias can be asymptomatic, especially small hernias. Larger hernias may cause symptoms such as:
- Heartburn, acid reflux, and indigestion
- Chest pain or discomfort
- Shortness of breath
- Pain or discomfort in the abdomen
- Complications:Untreated diaphragmatic hernias can lead to serious complications, including:
- Strangulation:The hernia can become trapped and cut off blood supply to the affected organs.
- Obstruction:The hernia can obstruct the passage of food and fluids through the digestive tract.
- Infection:The hernia sac can become infected.
- Respiratory problems:Large hernias can compress the lungs and impair breathing.
Preoperative Considerations
Preoperative assessment and evaluation are crucial for successful diaphragmatic hernia repair. A thorough history and physical examination help identify the type of hernia, associated symptoms, and any underlying medical conditions that may impact the surgical plan.
Patient preparation involves fasting for 8-12 hours before surgery to minimize the risk of aspiration during anesthesia. Anesthesia is typically general, ensuring complete relaxation and pain control throughout the procedure.
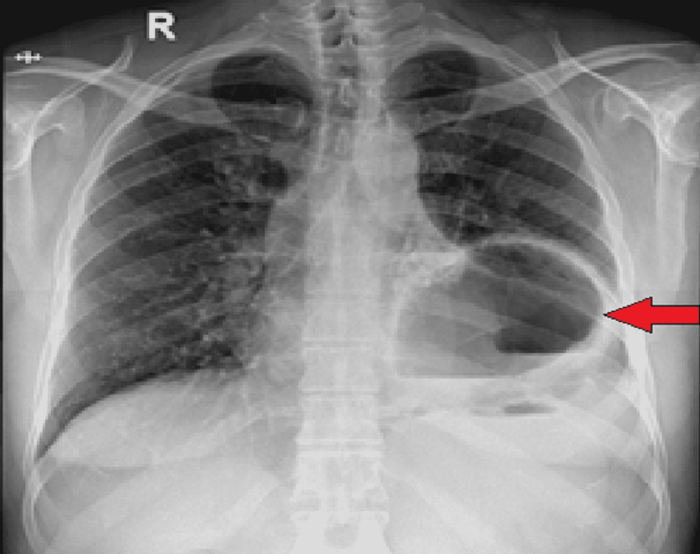
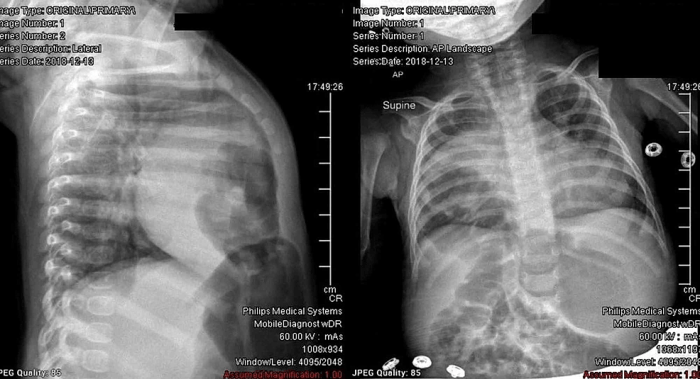
Imaging Studies
Imaging studies play a vital role in preoperative planning. Chest X-rays provide an initial assessment of the hernia size and location. Computed tomography (CT) scans offer detailed cross-sectional images, allowing for precise evaluation of the hernia contents, diaphragmatic defects, and surrounding structures.
Surgical Techniques

Surgical repair of a diaphragmatic hernia involves various approaches, including open, laparoscopic, and robotic techniques. Each approach offers unique advantages and considerations.
The choice of surgical technique depends on several factors, such as the size and location of the hernia, the patient’s overall health, and the surgeon’s experience and preference.
Open Approach
The open approach involves making an incision directly over the hernia. This allows for direct visualization and manipulation of the hernia, providing greater precision during repair.
- Incision placement varies depending on the location of the hernia.
- The hernia is reduced, or pushed back into its proper position.
- The diaphragmatic defect is closed using sutures or a mesh patch.
Laparoscopic Approach
The laparoscopic approach involves making several small incisions in the abdomen. A laparoscope, a thin tube with a camera, is inserted through one incision, providing a magnified view of the surgical field.
- The hernia is reduced using laparoscopic instruments.
- The diaphragmatic defect is closed using sutures or a mesh patch delivered through the laparoscopic ports.
- This approach offers less postoperative pain and a shorter recovery time.
Robotic Approach
The robotic approach combines the benefits of both open and laparoscopic techniques. A robotic system is used to manipulate laparoscopic instruments, providing enhanced precision and dexterity.
- The robotic approach offers the advantages of laparoscopy, such as reduced pain and recovery time.
- It also provides the surgeon with greater control and precision during the repair.
Postoperative Care: Cpt Code Diaphragmatic Hernia Repair
Postoperative care following diaphragmatic hernia repair focuses on pain management, wound care, and activity restrictions. Adequate pain control is crucial to ensure patient comfort and facilitate early mobilization. Wound care involves monitoring the incision site for signs of infection and ensuring proper healing.
Activity restrictions are necessary to prevent undue strain on the repair site and promote optimal recovery.
Potential Complications
Potential complications after diaphragmatic hernia repair include:-
- Infection
- Bleeding
- Hernia recurrence
- Phrenic nerve injury
- Gastrointestinal complications (e.g., nausea, vomiting, constipation)
Early detection and management of these complications are essential to minimize their impact on patient outcomes.
Recovery and Follow-Up, Cpt code diaphragmatic hernia repair
The expected recovery timeline after diaphragmatic hernia repair varies depending on the size and location of the hernia, as well as the patient’s overall health. Most patients can expect to return to normal activities within 4-6 weeks. Follow-up appointments are typically scheduled at regular intervals to monitor the healing process and assess for any complications.
Outcomes and Prognosis
The success rate of diaphragmatic hernia repair is generally high, with most patients experiencing significant improvement in their symptoms. Studies have reported success rates ranging from 85% to 95%, with recurrence rates typically below 5%.
Factors Influencing Outcomes
Several factors can influence the outcomes of diaphragmatic hernia repair, including:
- Hernia size:Larger hernias are more challenging to repair and may have higher recurrence rates.
- Surgical approach:Open surgery has traditionally been the preferred approach, but laparoscopic and robotic techniques are becoming more common. Laparoscopic repair may offer advantages in terms of reduced pain, shorter hospital stays, and faster recovery.
- Patient comorbidities:Patients with underlying health conditions, such as chronic lung disease or heart failure, may have a higher risk of complications and poorer outcomes.
Long-Term Prognosis
Most patients who undergo diaphragmatic hernia repair have a good long-term prognosis. However, potential complications can occur, including:
- Recurrence:The hernia may recur in a small percentage of patients, requiring additional surgery.
- Gastroesophageal reflux disease (GERD):This condition can develop after hernia repair, especially in patients with large hernias or those who have undergone open surgery.
- Dysphagia:Difficulty swallowing may occur in some patients after hernia repair, particularly those with large hernias or those who have undergone open surgery.
Regular follow-up care is important to monitor for any potential complications and ensure optimal long-term outcomes.
Special Considerations
Diaphragmatic hernia repair in specific patient populations requires specialized approaches.
Infants and Children
Infants and children with diaphragmatic hernias often have associated congenital anomalies. Surgical repair is typically performed through an abdominal or thoracoabdominal approach. The timing of surgery depends on the severity of the hernia and the presence of other anomalies.
Elderly Patients
Elderly patients with diaphragmatic hernias may have additional medical conditions that increase the risk of complications. Preoperative evaluation should include a thorough assessment of comorbidities and optimization of medical management.
Recurrent Diaphragmatic Hernias
Recurrent diaphragmatic hernias occur in approximately 5-10% of patients after initial repair. Risk factors include technical issues during the initial surgery, underlying neuromuscular disorders, and increased intra-abdominal pressure. Management involves re-exploration and reinforcement of the diaphragmatic closure.
Minimally Invasive Techniques
Minimally invasive techniques, such as laparoscopic and robotic-assisted surgery, are increasingly used for diaphragmatic hernia repair. These techniques offer advantages of reduced postoperative pain, shorter hospital stays, and improved cosmetic outcomes. However, they require specialized training and may not be suitable for all patients.
Questions and Answers
What are the common symptoms of a diaphragmatic hernia?
Symptoms may include chest pain, shortness of breath, abdominal pain, and difficulty swallowing.
How is a diaphragmatic hernia diagnosed?
Diagnosis typically involves a physical examination, imaging studies such as X-rays or CT scans, and upper gastrointestinal endoscopy.
What are the risk factors for developing a diaphragmatic hernia?
Risk factors include obesity, chronic coughing, heavy lifting, and trauma.